We can all agree that our children are the most important things in our lives. We would do anything for them, go full on mama bear to protect them. Cuts, scrapes, bruises—we bandage it all! We can solve almost any problem thrown at us.
 But what happens when the signs aren’t outward and obvious? We keep saying, “kids are resilient,” and while our children are resilient, they need our help to withstand the storms, especially the storm of 2020, which has led to increases in childhood and teenage depression and suicide.
But what happens when the signs aren’t outward and obvious? We keep saying, “kids are resilient,” and while our children are resilient, they need our help to withstand the storms, especially the storm of 2020, which has led to increases in childhood and teenage depression and suicide.
The following are several proactive strategies from licensed counselors that could help your child’s mental health.
Name feelings
It is OK for your child to experience BIG emotions. Have you met a toddler? Name those feelings! We name everything else for toddlers, “Don’t hit, use your words!” But sometimes, we forget to give them the actual words. Print off pictures of faces showing different emotions and put it up somewhere where your child can see. Refer to it when your child is showing a particular emotion. Let them see what their face does when it is upset, or angry, or even excited.
Don’t just help your toddlers, help your older kids name their feelings, too. Begin to help them recognize what their feelings are so they know what those emotions feel like. “Sadness makes my body feel…but it goes away when I…” or “Excitement makes my body feel…things that make me excited are…”
Shut up and LISTEN!
We adults talk…a lot. And often about random things that have more to do with “when I was your age” than to do with the actual situation. We try to fix our kids’ problems instead of just listening. Don’t tell them how to solve it; instead, ask if they even want your help or if they just need someone to bounce ideas off of.
Help them see if it is a “puddle,” “pond,” or “ocean” problem. With puddle problems, we can jump over and move on. With pond problems, we may need a boat to cross (in other words, help). With an ocean problem, we are going to need a much bigger boat and extra skills (a.k.a. LOTS of help and possible intervention).
To get discussion started, you can use conversation cards at dinner. If you are a busy family, play games in the car on the way to the ball field that get them talking. Would you rather? and Two highs and a low are some of our to-gos. You can find family question books on Amazon. They even have conversation napkins.
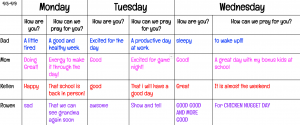
Here’s a check-in option I use with my 4th and 6th grader!
Make sure your child has a person.
Relationships are key. Every kid needs a person. As they grow into teenagers, their person may not be you, Mom, and that’s OK. An adult who checks in on them, who they trust, and who they share things with is a key support system that growing kids need.
If you begin to get concerned, look at whether there are changes in the way they think, feel, or act. As we move through Children’s Mental Health Awareness Month, the Mayo Clinic has some great resources to use if you suspect any changes in your child. It can be difficult to tell the difference between normal teen angst and what is actually depression. The important thing is to remember that depression comes even for the young.
Use the following lists to help keep your child safe
(Please remember that these are not complete lists and that all children are different and may respond to depression differently)
Emotional Changes:
- crying spells for no apparent reason
- frustration or feelings of anger, even over small matters
- irritable or annoyed mood
- loss of interest in or conflict with family and friends
- low self-esteem
- fixation on past failures or exaggerated self-blame or self-criticism
- ongoing sense that life and the future are grim and bleak
- frequent thoughts of death, dying, or suicide
Behavioral Changes:
- tiredness or loss of energy
- insomnia or sleeping too much
- change in appetite
- slowed thinking, speaking or body movements
- social isolation
- poor school performance or wanting to be absent
- less attention to personal hygiene or appearance
- self harm-burning, cutting, excessive piercing or tattooing
- angry outbursts, disruptive or risky behavior
- making a plan or attempting suicide
Remember to keep talking to your child(ren) and always have communication lines open. If you notice that signs and symptoms continue or cause you to have concerns about suicide or their safety, consult a doctor or mental health professional who is trained to work with kids and adolescents. Depression isn’t something that gets better on its own and may get worse if it goes untreated. Even if you don’t think the signs are severe, it’s OK to consult your physician or even reach out to your child’s teachers.
Mental Health Resources:
National Suicide Hotline 800-273-8255 or text HOME to 741-741
Mindfulness /Coping Strategies
- https://www.therapistaid.com/worksheets/family-mindfulness-schedule.pdf
- https://www.therapistaid.com/worksheets/progressive-muscle-relaxation-script.pdf
- https://www.therapistaid.com/interactive-therapy-tool/ocean-breathing-audio/active
- https://www.therapistaid.com/worksheets/coping-skills-anxiety.pdf
Remember that your mental health is important too, Momma. If the plane is going down, you put on your oxygen mask first. The same applies here. Doing what you can to make sure you are at your best will allow you to be a stronger support for your children, so they can live their best lives.